Most people with COVID-19 infection will never have to see a provider during their illness. In a world of self-testing and telehealth appointments, it's normal to wonder if you are okay at home. It can be scary to know that COVID can lead to more severe problems.
How do you know if you have severe COVID?
COVID infection can make you feel very sick even when you are not in any real danger of progressing to life-threatening illness. It can be hard to know when it's time to get further medical attention. COVID can cause severe symptoms like difficulty breathing that causes low oxygen levels in your body if this happens you will need to seek medical attention and supplemental oxygen.
How will you know if your oxygen level might be low?
• It will feel like you're working really hard to breathe.
• It may feel like you can't catch your breath.
• You may be having severe chest pain or tightness.
• You have a bluish or dusky color to your skin lips or nails.
• You might start to seem confused or disoriented.
• You may be having difficulty staying awake.
• If you're used to feeling short of breath with conditions such as asthma or COPD, you need to pay extra attention if you get COVID infection. These symptoms may worsen your baseline.
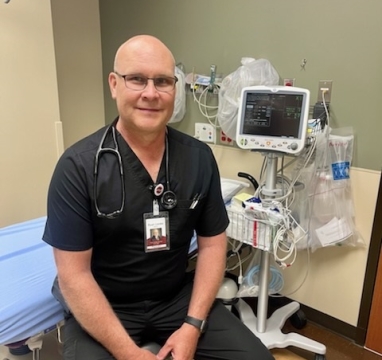
Emergency Services medical provider Ryan Lieske, PA-C, said “You should always go to the emergency department if you are experiencing chest pain.”
What risk factors may put me at risk for severe disease?
• Age over 65
• Diabetes
• Obesity
• Moderate or severe asthma
• Cancer
• Heart disease
• HIV
• Treatment with immunosuppressant drugs after an organ transplant
• Steroid use
• Not being vaccinated against COVID
Lieske suggests that if you feel like you are getting worse day-to-day, reach out to your health care provider. Be sure to contact their medical office before showing up so that they are alerted to your illness. If you are getting severely worse not being able to breathe or feeling confused, you may need to go to the emergency department.
“Your primary care provider may be able to prescribe outpatient antiviral medications to prevent you from getting worse,” said Lieske. “You may consider getting yourself a pulse oximeter to measure your oxygen level. If your oxygen levels are dropping consistently below 90% it may be time to go to the ER.”
Lieske shared that in the emergency department, the team will typically check your oxygen level with pulse oximetry, check your breathing rate, your heart rate, and your blood pressure. Depending on how your body is responding to the infection, they may do some additional testing such as an X-ray of your lungs, a CT scan to look at your lungs, an EKG of your heart to look at the strain on your heart, and additional blood tests to make sure that your other organs are functioning properly. Based on these results they determine whether you can continue to recover at home or stay in the hospital for closer monitoring.
You will likely need to stay in the hospital:
• If you are struggling to breathe and your oxygen levels are low
• If you are not able to stay hydrated and are not tolerating fluids
• If you are confused, excessively sleepy, or not very coherent
• If you have medical issues that may make it more likely that your infection will worsen
“If these are apparent you may be admitted to monitor your symptoms more closely,” said Lieske. “Inpatient hospital treatment may include oxygen, IV fluids, steroids, and antiviral medications.”
Important things to remember
Severe COVID infection may be indicated by difficulty breathing, confusion, disorientation, and bluish discoloration of the lips or hands.
Lieske said, “Keep in mind most people with COVID infection do not need to go to the hospital and can recover smoothly at home.” He added, “In the emergency room we can check your vital signs and run some tests to see if it is safe for you to go home or if you need to stay in the hospital.”